The surgery
So here I am, nearly 11 weeks post-surgery. I spent a month in Sydney and ended up having major surgery. They did a thoracotomy (a cut under the shoulder blade to access the mesh in my chest wall), removed the old mesh, shaved a bit more of my ribs, cleaned everything out, and rebuilt my chest wall with two new pieces of mesh and titanium staples. It was intense.
I found my surgeon, Dr Fenton-Lee, through a chain of events that actually started on TikTok. I commented on a woman’s post where she’d had a recurrence and was getting treatment at the Chris O’Brien Lifehouse in Sydney. I’d never heard of it, so I started researching. I called, got recommended a doctor, grabbed a pad and paper, wrote down names, made more calls, and took more notes. That eventually led me to Dr Fenton-Lee, who specialises in mesh removal.
At the same time, I’d been accepted into a public hospital in Melbourne. It was basically a race to see who could get me in first.
Melbourne was looking promising, and then out of nowhere, the day before my appointment, they moved it a month. I emailed and got no reply.
They’d asked me to get a CT and X-ray done. In that CT they found a mass on my liver, so then I had to go to Perth for two MRIs: one for my liver and one for my chest wall. That second one had to be rescheduled because my flights the month before were cancelled. Nothing is easy when you live 700km from the city and there’s barely any support for rare cases out in the country. Thankfully, the liver ended up being okay, but it now needs ongoing monitoring.
While I was in Perth, the Sydney surgeon called and gave me a tentative date. It wasn’t going to be simple. They wanted three surgeons involved: my main surgeon, a cardiothoracic surgeon, and a plastic surgeon. The clinic manager told me it would take time to organise. I can see both sides. The complexity is huge, but as a patient, my life had already been on hold for over a year. I finally had some traction, but I couldn’t push too hard, and I had to prepare my family to drop everything the moment we got the call. When the date finally came through, I couldn’t even feel excited, I just had to accept it and go.
We booked flights and headed to Sydney in early September. They told me I needed to come in the night before surgery. We had a couple of days to get organised, and of course, it wasn’t smooth. They wanted my echocardiogram from six months earlier, but the clinic wouldn’t release it to me. So I spent hours on calls and emails trying to sort it and honestly, the system makes you feel like no one really cares.
Then I got a call saying my surgery wouldn’t go ahead because I was from WA, and a hospital manager had overruled my surgeon. There was a whole fight happening behind the scenes, and I just had to hope they would sort it out.
When I arrived at the hospital, there was no bed for me. By the time they finally found one that night, there was an influenza A outbreak on the ward, and at 9:30pm they moved me from a single room into a room with three men.
All three doctors came to see me, asked questions, poked around, and checked everything. I still had no idea what was going to happen. I was scared, nervous, and going into a surgery where even the team didn’t fully know what they would find. Nothing felt smooth. I just had to let go and trust these doctors I’d only just met in person.
That night was one of the worst hospital nights I’ve ever had. I was in a room with three men and two of them kept me awake all night. I honestly didn’t know where I was, it felt like a crazy psych ward. The old man across from me talked for hours about how he wasn’t having an MRI. It took me a while to realise he was talking to himself. By midnight he was yelling and the nurses had to give him something to settle him.
Another man had his light on, phone on loud, laughing at videos, and then at 3am he got on the phone having a huge argument with his mum for over an hour. The guy beside me finally yelled “that’s enough!” at 5am.
I went out to the couch a few times to try to rest, but that was scary as I didn’t want to get influenza right before surgery. By the next day, I was wrecked. No sleep, no information, no idea what was happening. No one knew what time I needed to be ready. They just told me not to eat or drink. I asked a few times, but I didn’t want to make a fuss in case I got kicked out of the bed they had finally given me.
At 12pm an orderly walked in and started wheeling my bed. I asked what was happening and she just said, “It’s surgery time.” I only had a moment to message my husband and mum saying, “Going to surgery.” I didn’t know where to put my phone or my things, and honestly, she didn’t care.
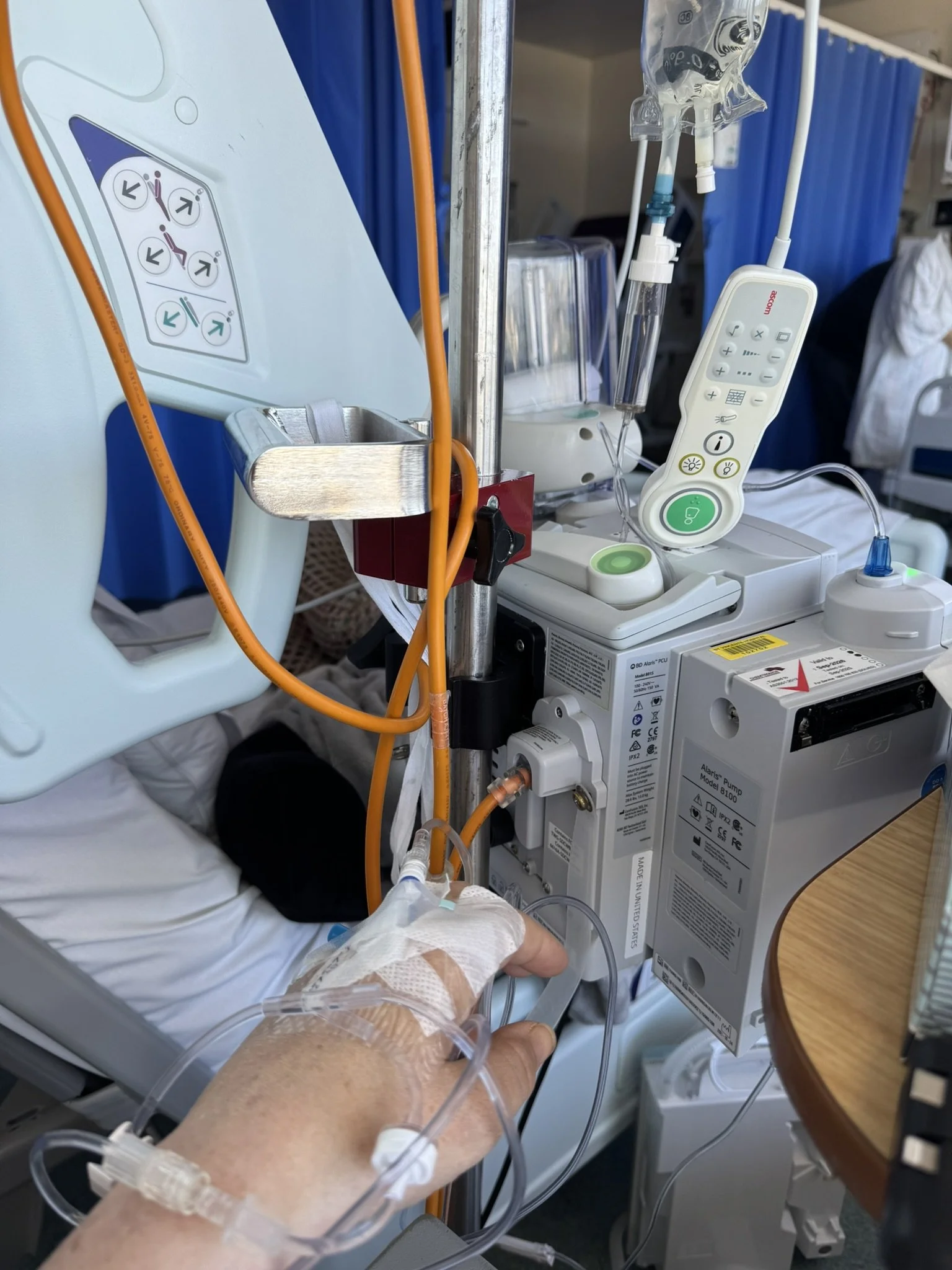
They took me to theatre and started putting in cannulas, which is always hard for me because I have no decent veins. She insisted on going through my wrist which is painful, but she shoved in some local and there was no messing around. By the time they prepped me, I couldn’t stop the tears. I had planned to go in calm, do some breathing, but the truth was I was terrified.
I woke up at 6:30pm in the ICU. I had nine tubes coming out of me, and I couldn’t move. The pain was extreme. I had no idea what had happened in surgery. I felt really nauseous and kept asking for something to nibble on, but they just gave me more anti-nausea meds through the cannula.
Over the next couple of days I slowly pieced together what had been done. It was the full reconstruction, so I knew I was in for a rough couple of months.
My husband and kids visited me in ICU and there’s one memory that still breaks my heart. I started getting nauseous again, and I was crying, begging them for something tiny to nibble on so I didn’t vomit. They weren’t listening and I started dry-reaching, which was awful in the state I was in. My son saw me like that. Once I realised the anti-nausea meds weren’t working for me, I kept a little stash of food so I could nibble and keep the nausea away myself.
After a couple of days I was moved to a ward, thank goodness not Ward 7. I do have a funny memory though. They gave me two tapentadol and I was absolutely off my face, telling the nurses my whole experience in Ward 7 and making them laugh.
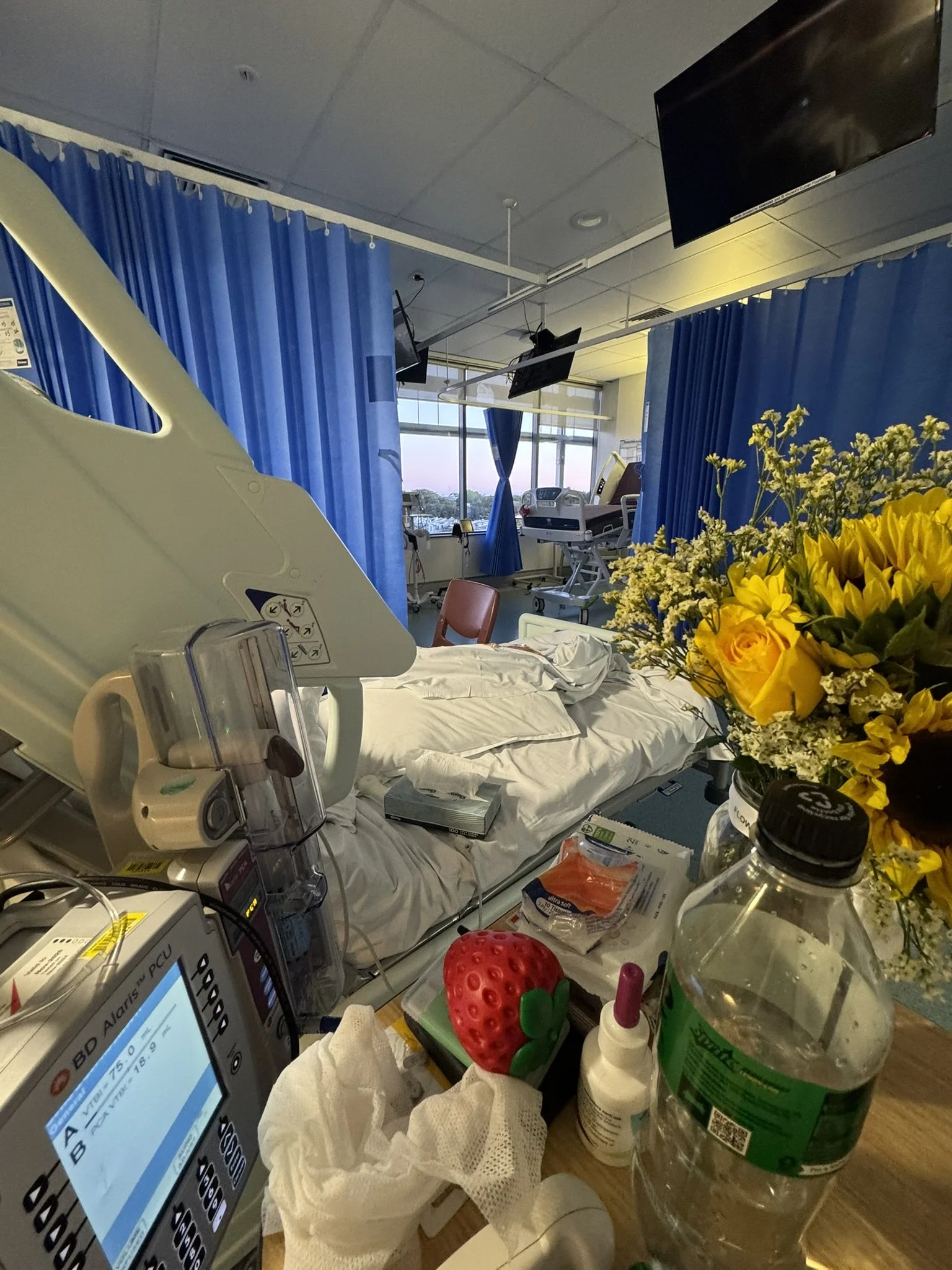
I ended up in Ward 10, a high-needs ward with people who had major chest surgeries and even heart transplants. It was not for the faint-hearted.
I spent the next eight days in that ward, most of the time stuck behind a blue curtain. You don’t realise how much you need to see outside until you can’t. It affects your mental health more than you think. The tubes slowly came out one by one, but I was left with one in my chest wall right up until the last night. The drain in my lung was the worst, I could feel it constantly, no matter how many painkillers I had. When they finally pulled it out, I was shocked at how long it was, all coiled up inside my lung.
Lung pain is no joke. When the mucus started coming up and I tried not to cough, I choked and couldn’t breathe. They gave me nebulisers a few times to help break it down. Not being able to move or do anything for yourself is such a degrading feeling. I hate asking for help, but I had no choice. I went a couple of days without a wash or brushing my teeth because the ward was so chaotic and I didn’t want to ask anyone or try to move.
By Friday, the veins in my hand started giving out. I kept saying it wasn’t working and it was hurting, but no one listened. The pain specialist jammed something in on Saturday morning and my hand blew up. The cannula had to come out, but I still had the chest drain in, so I needed another one for pain relief. They decided to trial me on oral meds, but by lunchtime it was clear they weren’t helping.
I had a very young nurse that day, and I kept telling her I wasn’t okay. She just said, “You’ve had major surgery and still have a tube in, you need to expect pain.” By 1pm I was in 10 out of 10 pain, worse than childbirth. It felt like giving birth out of my chest wall, except it was constant. I was moaning and crying; I think I blocked parts of it out. Even writing this now, the tears come because the memory is still so raw.
When the nurse shift changed, the new nurse took one look at me and jumped straight into action. They started arguing about protocol and how I shouldn’t have had my cannula removed (even though it burst). The emergency doctor arrived around 3 pm, and the only veins left were my wrist (which is painful) or a tiny one at the end of my hand. He got it first go, and within half an hour, the pain was finally under control. It was a day I never want to relive. It shook me and I felt invisible and ignored.
The Saurday from hell - from 10 out of 10 pain to high as a kite.
I know big hospitals are overwhelmed, understaffed and stressful places, but it felt like no one was listening to the patients. It was a multicultural hospital with nurses from everywhere, and there was a lot of tension and bickering between them. I kept trying to stay positive and remind myself I had an incredible surgeon, and that this was temporary.
By day 12, they finally removed the chest wall drain. I was free and able to go to the toilet on my own, shower on my own, brush my teeth whenever I wanted, even make myself a cup of tea. Even now, 11 weeks later, I still feel excited about having my independence back after losing it for what felt like forever. Fresh air, sunlight, even just watching the clouds, all feel different now. I don’t take any of it for granted.
In my last two nights, I had Australian nurses, and everything felt calmer. I got proper showers and they treated me like a human. Somewhere in all this, Dale and the kids had to fly home, and Mum came to take over helping me. It was still hard not knowing what recovery would look like or when I could get back to Esperance, but the only way was forward.
I eventually found out they replaced the old mesh with new mesh. I wasn’t thrilled about that, but seeing my surgeon two weeks later, he explained there was no choice, the space was too large to leave. We still don’t fully know what caused my chronic pain. You could see the chest wall sinking in. One report said the old mesh was “grossly thickened.” One thought it was a hernia. Others found neuromas in the mesh. It was a huge risk, and no one knew how I’d come out the other side.
But now, I truly believe it was worth it. I have more energy than I’ve had in a year and a half. I still have wicked nerve pain and sleep isn’t easy, but it’s nothing compared to what I lived with before.
Mum and I spent just over two weeks in Sydney waiting for the all-clear to go home. We moved to Bondi for a week and loved being close to the ocean. I had to walk every day to get my lung function back, and when my X-ray finally looked good enough, I was cleared to fly home.
Coming home was so exciting. Being surrounded by friends and family, there’s honestly no place like home.
And now I’m on a mission to help other people living with chronic pain or stuck in the system. By sharing my story, I want to show how important it is to advocate for yourself. Do everything you can. Don’t take no as the end.
Through all this, I’ve also become a consumer on multiple cancer research grants, and I love hearing what’s happening in the field. I hope new technology they are working on and new approaches can help shift our system away from gaslighting and dismissal, and back toward treating people like humans.
If you made it this far, thank you.
And please remember: your health truly is your greatest wealth. Look after yourself.